Case Description
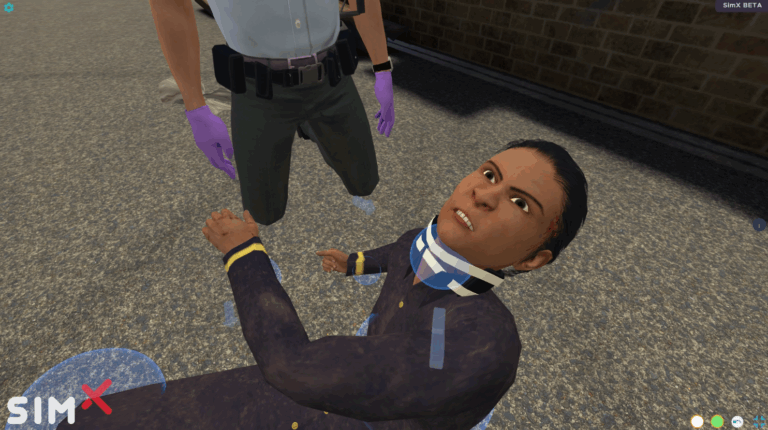
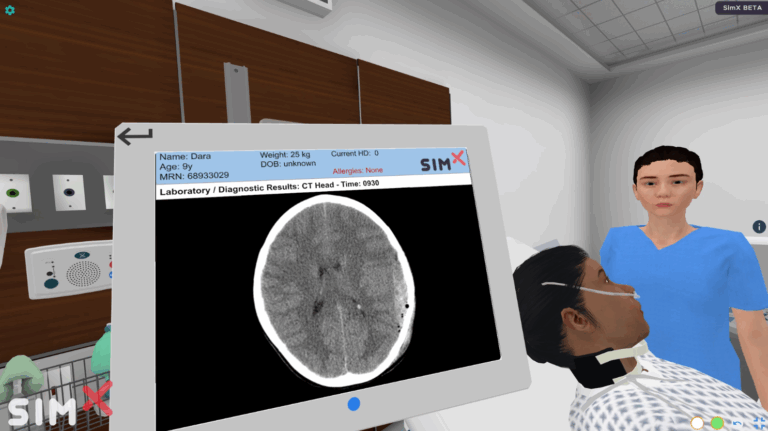
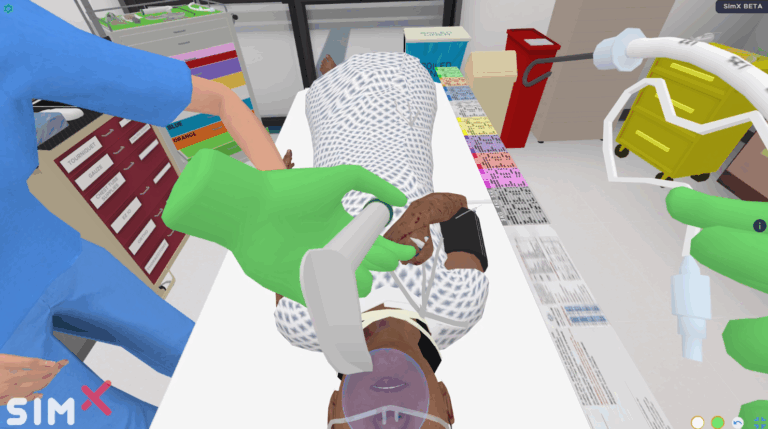
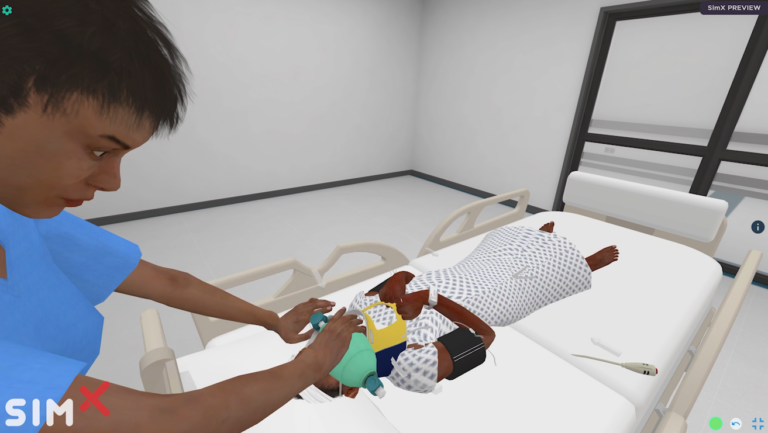
A 9-year-old is evaluated after a traumatic injury. The trainee must stabilize the patient in a hospital-based environment. On arrival, the child appears agitated. Their exam is remarkable for superficial scrapes and a left arm fracture. The patient’s head is covered, hiding a significant scalp wound. After completion of the primary survey, the child becomes altered with incomprehensible speech. The learner should recognize decline and consider airway protection. The patient should have a head CT which shows a left-sided epidural hemorrhage. Neurosurgery should be consulted. The team must medically manage the patient’s increased intracranial pressure until Neurosurgery is able to drain the hematoma in the operating room. If there is a delay in management, the patient’s neurologic status will decline progressing to absent speech, absent eye opening, and decorticate posturing. If the trainee does not recognize the decline, the patient will progress to full brainstem herniation, demonstrating blown pupil, flaccid paralysis, and loss of all brainstem reflexes.
The case resumes after the patient returns from the OR for surgical evacuation and EVD placement. Shortly after arrival, the patient becomes tachycardic and develops right arm twitching with leftward eye deviation. The learner should identify the seizure and give appropriate anti-epileptic medications.
Learning Objectives
1. Learner consults interpretive services when required for patients that are not English speaking. Learner should use the interpreter appropriately, speaking directly to the patient in short
phrases.
2. Learner applies monitors, protects c-spine, and obtains IV/IO access.
3. Learner completes the primary survey or MARCH.
a. Identifies and treats any massive hemorrhage.
b. Evaluates the airway with cervical spine control.
c. Evaluates breathing/respiration.
d. Evaluates circulation.
e. Evaluates disability/hypothermia/head injury using AVPU.
f. Exposures the patient while preventing hypothermia.
4. Learner recognizes pediatric abnormal vital signs.
5. Learner appropriately doses medications for a pediatric patient.
6. Learner recognizes neurological decline.
7. Learner recognizes the need for airway protection when GCS <8.
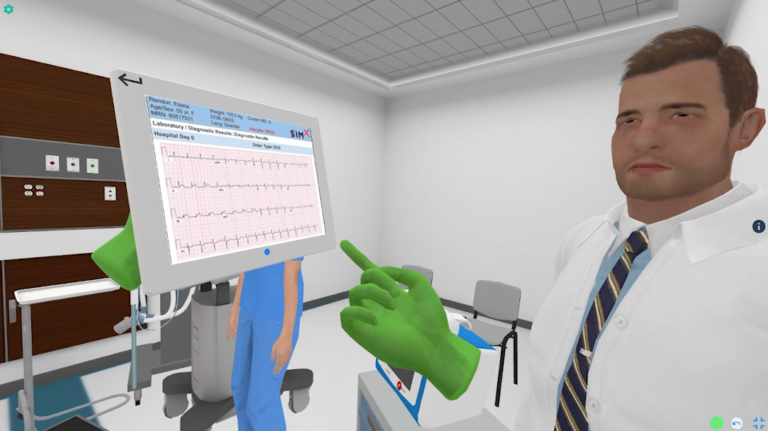
8. Learner recognizes the need for head CT.
9. Learner considers intracranial injury causing the patient’s decline.
10. Learner consults neurosurgery or initiates transfer if unavailable.
11. Learner applies best practice guidelines for TBI management.
a. Gives 3% saline bolus or mannitol.
b. Raises HOB to 30 Degrees.
c. Performs hyperventilation to EtCO2 ~35 mm Hg if acutely herniating.
d. Ensures adequate sedation and pain control.
e. Gives levetiracetam for seizure prevention.
f. Prevents secondary injury.
i. Maintains normothermia.
ii. Maintains normotensive to permissive hypertension.
iii. Avoids hypoxia and hyperoxia.
iv. Maintains ETCO2 35-45.
v. Maintains euglycemia.
vi. Treats any active seizures.
12. Learner recognizes traumatic seizure and gives a benzodiazepine.
MINIMUM:
OS: Windows 10
Processor: Intel Core i5-2300 | AMD FX-4350
Memory: 4 GB RAM
Graphics: Nvidia GeForce GTX 2060
DirectX: Version 11
Storage: 12 GB available space
RECOMMENDED:
OS: Windows 10
Processor: Intel Core i7-2300 | AMD FX-4350
Memory: 8 GB RAM
Graphics: Nvidia GeForce GTX 3060
DirectX: Version 11
Storage: 12 GB available space
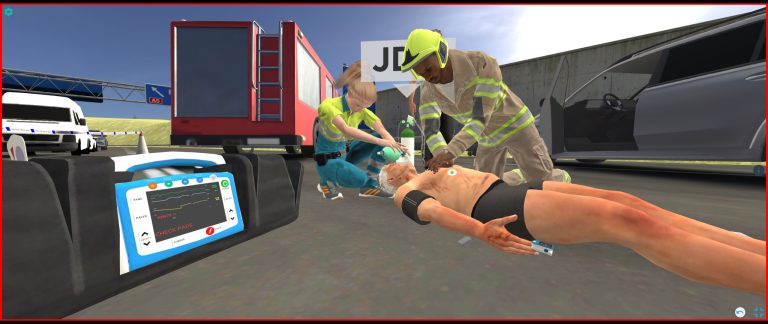
Interested in this scenario?
Sign up to talk with a member of the SimX team today!