What’s New? The release of SimX 25r1 includes a variety of new content, features, and updates that are aimed at...
SimX 2025 Release 1

What’s New?
The release of SimX 25r1 includes a variety of new content, features, and updates that are aimed at enhancing your overall experience with the SimX platform. These additions and improvements include In-Headset Safety Warnings, Virtual BATDOK Enhancements, Custom Scenarios, Translations, and more.
Features
In-Headset Safety Warnings
SimX’s new 25r1 software update prioritizes user safety by including a mandatory in-headset virtual reality (VR) health and safety acknowledgement. This measure ensures that all users are aware of potential health and safety risks before engaging in any VR scenario, promoting a safe VR experience for all SimX users.
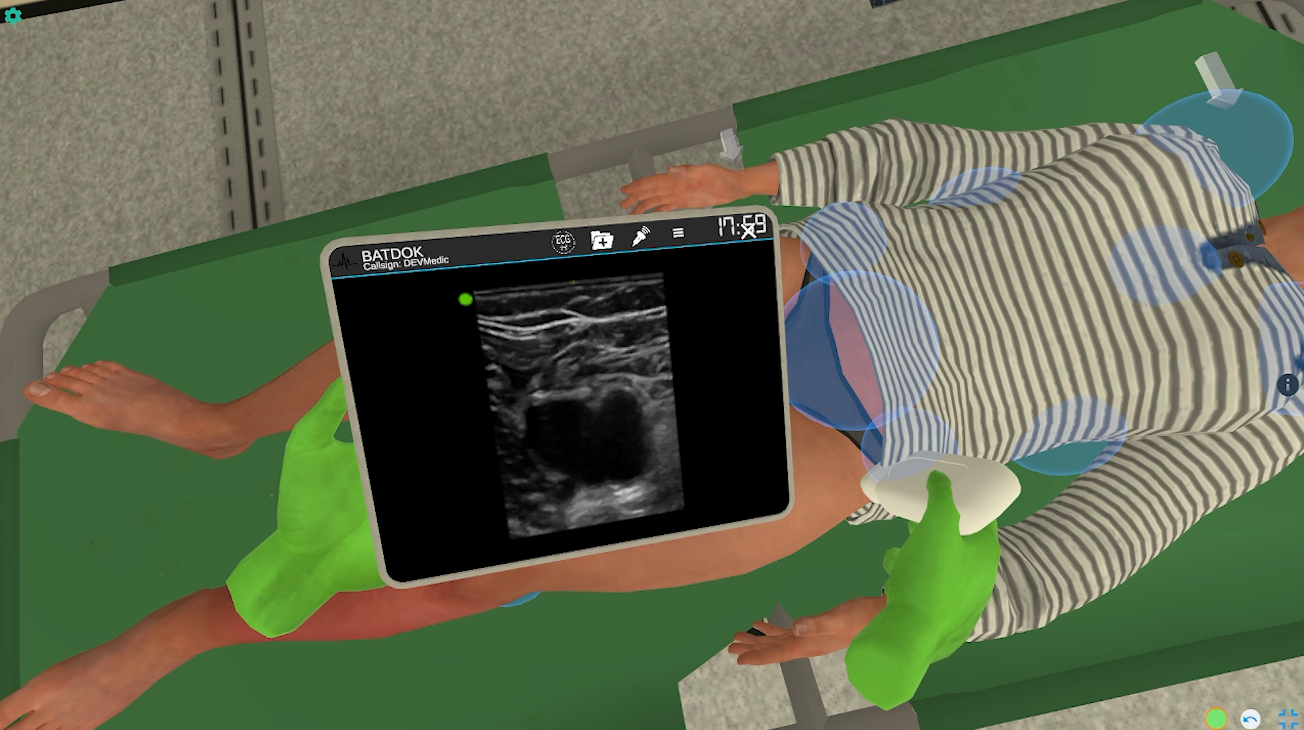
Virtual BATDOK Enhancement: Prolonged Casualty Care & Small Unit Care Capabilities
We’ve expanded the virtual BATDOK mobile medical documentation tool to support Prolonged Casualty Care (PCC) and Small Unit Care (SUC) scenarios. Previously, the virtual BATDOK was focused on Tactical Combat Casualty Care (TCCC).
New BATDOK Features
- Prolonged Casualty Care (PCC) Capability Support – Added new functionality to document assessment findings, vital signs, and interventions during prolonged care scenarios.
- Real-time documentation of vital signs (HR, BP, Resp, Temp, SpO2, EtCO2).
- Visual trending of vital signs over time through a table and interactive graphs, allowing for quick assessment of patient status.
- Digital checklists for nursing care reminders and treatments, enabling users to track completed tasks.
- Easy check-off functionality with visual confirmation.
- A comprehensive log that records all documented vital signs, assessments, interventions, and treatments with timestamps.
- A new UI to calculate TBSA percentage of burns, with a visual representation of body areas and automatic calculation.
- Small Unit Care (SUC) Capability Support – Introduced a new SUC mode to support Small Unit Care-focused training scenarios.
- A dedicated interface for Small Unit Care scenarios, focusing on physical exam documentation relevant to austere environments.
- New physical exam flowsheet and small unit care functionalities to meet the unique needs of the SUC curriculum.
- SUC features are activated only for relevant scenarios to simplify the user experience.
UI/UX Improvements
- Streamlined user experience and interface by removing unnecessary submenu UX/UI elements to reduce cognitive load and enhance usability.
Custom Scenarios
Custom scenarios created between SimX 25r1 and the previous SimX release are now accessible in the SimX marketplace.
Difficult Client
Engage in a one-on-one conversation with Michael after he receives unexpected news about his involuntary hospital stay. This scenario challenges learners to navigate escalating behaviors while maintaining therapeutic communication and safety.
- Therapeutic Communication – Use effective techniques to manage patient distress and defuse tension.
- Behavioral Redirection – Set clear limits to guide interactions and prevent escalation.
- Safety Management – Recognize risks and implement appropriate safety precautions.
- De-escalation Techniques – Employ communication strategies to calm and reassure the client.
This scenario is authored by Georgian College. To learn more, see Difficult Client.
De-escalation of Agitated Patient
Manage an agitated 30-year-old female, Eleanor, who is brought to the emergency department by EMS with an unknown medical history. This scenario challenges RNs and APRNs to collaborate using an interdisciplinary approach to safely de-escalate the situation.
- Therapeutic Communication – Apply effective techniques to engage with an agitated patient and reduce distress.
- De-escalation Process – Navigate escalating behaviors while maintaining a calm and controlled environment.
- Safety Awareness – Identify and implement strategies to ensure the safety of both the patient and healthcare providers.
- Focused Assessment – Conduct a physical assessment as appropriate given the patient’s agitation level.
- Interprofessional Collaboration – Communicate effectively in high-stress situations within the healthcare team.
- Medication Management – Assess the need for medication and administer it safely when appropriate.
This scenario is authored by College of St. Scholastica. To learn more, see De-escalation of Agitated Patient.
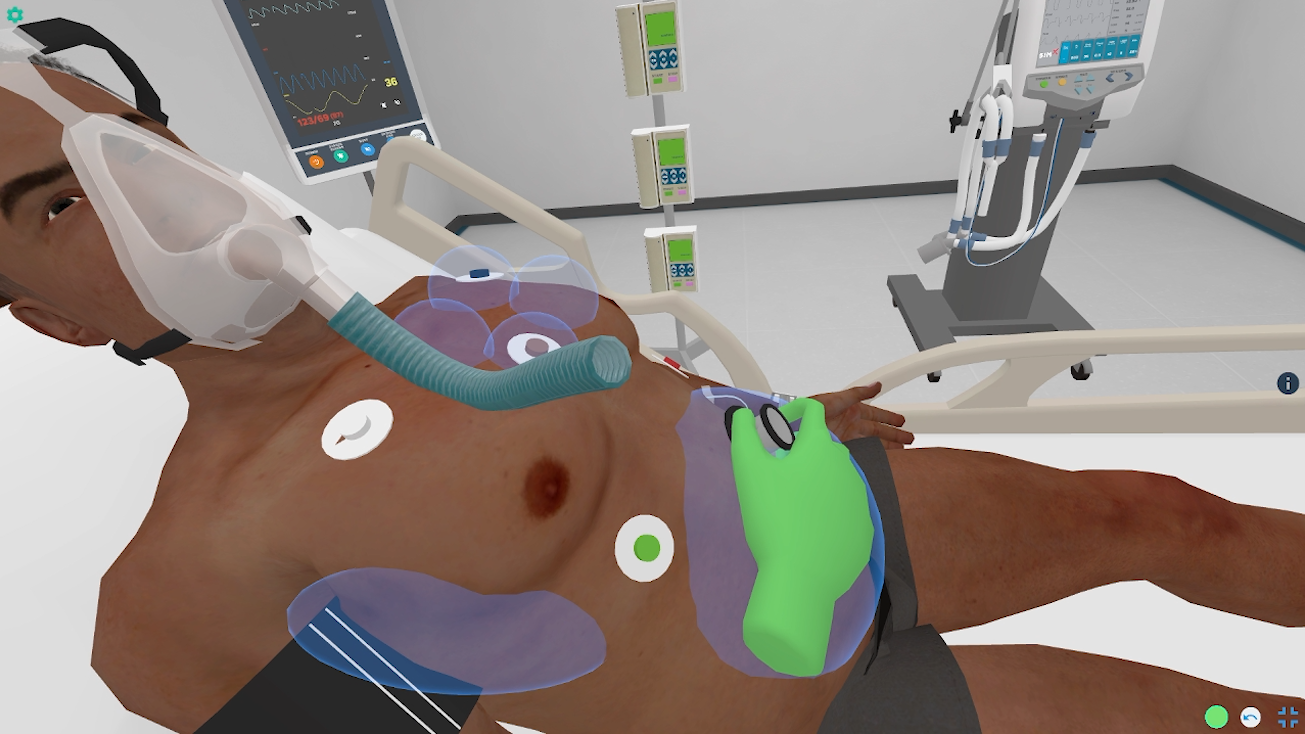
Rapid Sequence Intubation
A critically ill patient requires airway intervention in an emergency setting. Learners must evaluate the patient, select appropriate medications, and perform a safe and efficient RSI.
- Pre-Intubation Assessment – Identify indications and contraindications for RSI.
- Pharmacologic Management – Select and administer sedatives and paralytics.
- Airway Securement – Confirm successful intubation and ensure oxygenation.
- Complication Management – Recognize and respond to failed airway scenarios.
This scenario is authored by TriHealth. To learn more, see Rapid Sequence Intubation.
Management of Complications During Laparoscopic Surgery
A routine laparoscopic cholecystectomy turns critical when a patient develops an anaphylactic reaction and elevated peak airway pressures. Learners must respond to intraoperative complications in real time.
- Intraoperative Crisis Management – Recognize and address airway and circulatory emergencies.
- Team Coordination – Work effectively with surgical and anesthesia teams.
- Anaphylaxis Treatment – Identify symptoms and initiate emergency intervention.
- Ventilation Management – Adjust settings for patients with respiratory distress.
This scenario is authored by NYU Langone Health Department of Anesthesiology, Peri-operative Care, and Pain Medicine. To learn more, see Management of Complications During Laparoscopic Surgery.
Critical Care Post-MVA
A 33-year-old male presents after a motor vehicle crash with multi-system trauma. Learners must rapidly assess injuries, manage life-threatening conditions, and communicate effectively in a high-stakes environment.
- Primary Trauma Assessment – Follow ABC protocols to stabilize the patient.
- Resuscitation Management – Administer fluids, blood products, and critical interventions.
- Procedural Interventions – Perform airway management, chest decompression, and hemorrhage control.
- Interdisciplinary Teamwork – Coordinate with trauma teams for optimal patient outcomes.
This scenario is authored by Southeastern Illinois College. To learn more, see Critical Care Post-MVA.
Virtual Manikin™ — Outpatient Soft Skills
Practice patient-centered communication and soft skills in an ambulatory care setting. Learners engage with diverse virtual patients and adapt their approach accordingly.
- Dynamic Patient Interaction – Adjust communication style to different patient needs.
- Interdisciplinary Collaboration – Work with healthcare professionals to coordinate care.
- Cultural Competency – Practice interactions with patients from diverse backgrounds.
- Real-Time Scenario Customization – Modify case complexity and patient responses.
This scenario is authored by SimX. To learn more, see Virtual Manikin™ — Outpatient Soft Skills.
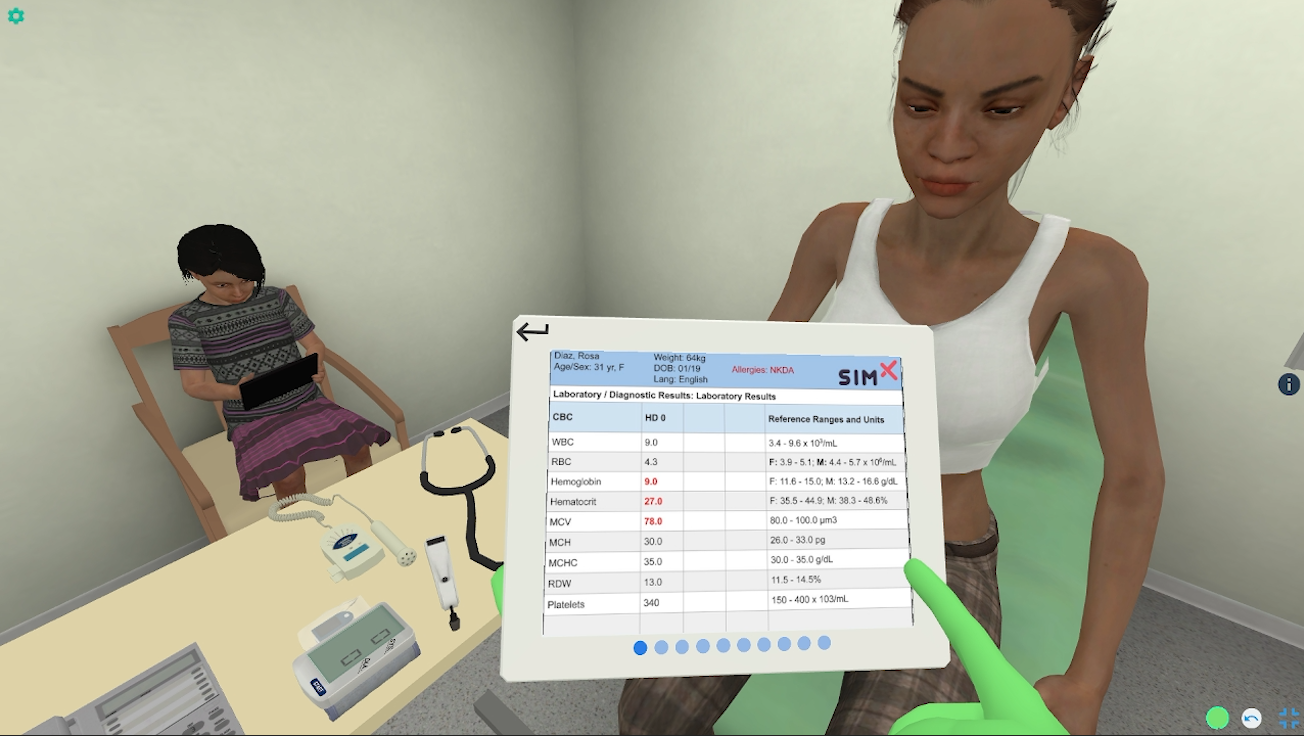
SDOH Food Insecurity, Women’s Health
A pregnant patient with gestational diabetes presents for routine prenatal care but reveals food insecurity concerns. Learners must integrate social determinants of health into their clinical decision-making.
- Comprehensive Patient Assessment – Identify SDOH factors affecting health outcomes.
- Nutritional Counseling – Provide guidance tailored to resource-limited circumstances.
- Interdisciplinary Resource Coordination – Connect patients with community support programs.
- Holistic Care Planning – Develop sustainable strategies for long-term wellness.
This scenario is authored by St. John Fisher University Wegmans School of Nursing. To learn more, see SDOH Food Insecurity, Women’s Health.
Pharmacotherapy of Endocarditis and Septic Shock
A patient with bacterial endocarditis deteriorates into septic shock. Learners must initiate timely pharmacologic interventions and support hemodynamic stability.
- Infection Identification – Recognize signs of endocarditis progression.
- Sepsis Resuscitation – Implement early goal-directed therapy with fluids and vasopressors.
- Antimicrobial Stewardship – Choose appropriate antibiotics based on culture results.
- Cardiovascular Monitoring – Manage shock states and prevent multi-organ failure.
This scenario is authored by University of Pittsburgh School of Pharmacy. To learn more, see Pharmacotherapy of Endocarditis and Septic Shock.
ICU Clinical Swallow Evaluation—Speech Pathology
Manage an agitated 30-year-old female, Eleanor, who is brought to the emergency department by EMS with an unknown medical history. This scenario challenges RNs and APRNs to collaborate using an interdisciplinary approach to safely de-escalate the situation.
- Therapeutic Communication – Apply effective techniques to engage with an agitated patient and reduce distress.
- De-escalation Process – Navigate escalating behaviors while maintaining a calm and controlled environment.
- Safety Awareness – Identify and implement strategies to ensure the safety of both the patient and healthcare providers.
- Focused Assessment – Conduct a physical assessment as appropriate given the patient’s agitation level.
- Interprofessional Collaboration – Communicate effectively in high-stress situations within the healthcare team.
- Medication Management – Assess the need for medication and administer it safely when appropriate.
This scenario is authored by University of Delaware College of Health Sciences. To learn more, see ICU Clinical Swallow Evaluation—Speech Pathology.
Establishing Vascular Access for Long-Term Antibiotic Therapy
A patient requiring long-term IV antibiotics presents for vascular access placement. Learners must select the appropriate site, perform the procedure, and ensure catheter maintenance.
- Site Selection & Preparation – Identify optimal vascular access sites based on patient needs.
- Aseptic Insertion Technique – Reduce infection risk with proper sterile protocols.
- Device Management – Ensure catheter patency and long-term functionality.
- Patient Education – Instruct on care, warning signs, and follow-up requirements.
This scenario is authored by CLINSPEC Solutions, LLC, CVC Health Care, LLC, and Precision Vascular, LLC. To learn more, see Establishing Vascular Access for Long-Term Antibiotic Therapy.
Establishing Vascular Access in a Difficult Intravenous Access Patient
A patient recovering from septic shock requires vascular access, but multiple IV attempts have failed. Learners must assess the situation and successfully establish access using advanced techniques.
- Patient Assessment – Identify challenges and determine alternative access strategies.
- Ultrasound Guidance – Utilize imaging to improve precision in line placement.
- Procedure Performance – Successfully place a midline catheter or alternative device.
- Documentation & Monitoring – Ensure post-procedure care and prevent complications.
This scenario is authored by CLINSPEC Solutions, LLC, CVC Health Care, LLC, and Precision Vascular, LLC. To learn more, see Establishing Vascular Access in a Difficult Intravenous Access Patient.
SUC Abdominal Pain (Small Unit Care Curriculum)
Assess and manage a patient presenting with abdominal pain in a clinic setting. Learners must conduct a focused history, perform an exam, and develop a differential diagnosis to rule out emergent conditions and determine next steps.
- Clinical Assessment – Gather a detailed history and perform a targeted physical exam.
- Differential Diagnosis – Identify potential causes and recognize red flags.
- Point-of-Care Testing – Utilize appropriate diagnostic tools to confirm or rule out urgent conditions.
- Evacuation & Referral – Decide whether the patient requires transport for higher-level care.
This scenario is authored by our VALOR Program. To learn more, see SUC Abdominal Pain.
SUC Cold-Related Illness (Small Unit Care Curriculum)
Respond to a patient experiencing altered mental status due to prolonged cold exposure. Learners must assess the severity of hypothermia, initiate rewarming techniques, and determine the need for transport.
- Hypothermia Recognition – Identify signs of mild, moderate, and severe cold-related illness.
- Critical Decision-Making – Differentiate between exposure effects and other medical conditions.
- Patient Stabilization – Implement rewarming and supportive therapy to prevent deterioration.
- Evacuation Planning – Coordinate safe transport for further medical intervention if necessary.
This scenario is authored by our VALOR Program. To learn more, see SUC Cold-Related Illness.
SUC Peritonsillar Abscess (Small Unit Care Curriculum)
A patient presents with worsening sore throat, difficulty swallowing, and a muffled voice. Learners must assess for airway compromise, diagnose peritonsillar abscess, and initiate appropriate treatment.
- Airway Assessment – Recognize signs of upper airway obstruction.
- Diagnostic Evaluation – Perform an oropharyngeal exam to confirm peritonsillar abscess.
- Treatment Strategies – Initiate antibiotics, drainage procedures, and supportive care.
- Evacuation Consideration – Determine whether emergency ENT intervention is required.
This scenario is authored by our VALOR Program. To learn more, see SUC Peritonsillar Abscess.
SUC Flank Pain (Small Unit Care Curriculum)
A patient presents with acute flank pain, requiring learners to rapidly assess, develop a differential, and decide on further testing. Learners must determine whether the pain is caused by nephrolithiasis, infection, or another urgent condition.
- Focused History & Exam – Assess for classic signs of renal pathology or systemic illness.
- Differential Diagnosis – Distinguish between urological, gastrointestinal, and musculoskeletal causes.
- Diagnostic Testing – Use point-of-care imaging and laboratory analysis for confirmation.
- Evacuation Planning – Decide if the patient requires further care or urgent transport.
This scenario is authored by our VALOR Program. To learn more, see SUC Flank Pain.
SUC Deep Venous Thrombosis (Small Unit Care Curriculum)
A patient presents with unilateral leg pain and swelling, raising concern for a deep vein thrombosis. Learners must evaluate risk factors, initiate appropriate diagnostics, and determine the best treatment approach.
- Risk Stratification – Assess patient history and presentation for thromboembolic risk.
- Diagnostic Evaluation – Recognize key clinical signs and order appropriate imaging when indicated.
- Treatment Initiation – Implement anticoagulation therapy and monitor for complications.
- Evacuation Consideration – Determine if hospitalization or specialty care is required.
This scenario is authored by our VALOR Program. To learn more, see SUC Deep Venous Thrombosis.
SUC Rhabdomyolysis (Small Unit Care Curriculum)
A patient complains of muscle weakness and dark urine following prolonged exertion. Learners must recognize the signs of rhabdomyolysis, order necessary lab tests, and initiate fluid resuscitation to prevent complications.
- History & Physical Exam – Identify risk factors such as exertion, trauma, or substance use.
- Laboratory Evaluation – Assess creatine kinase, renal function, and electrolytes.
- Treatment Protocols – Initiate IV hydration and monitor for acute kidney injury.
- Evacuation Planning – Arrange for hospitalization if necessary.
This scenario is authored by our VALOR Program. To learn more, see SUC Rhabdomyolysis.
SUC Snake Envenomation (Small Unit Care Curriculum)
A patient presents after a snake bite with localized pain and progressive swelling. Learners must assess the severity of envenomation, manage symptoms, and determine if antivenom is required.
- Bite Assessment – Differentiate between dry and venomous bites.
- Symptom Monitoring – Recognize progressive systemic effects such as neurotoxicity or coagulopathy.
- Antivenom Administration – Determine appropriate use of antivenom therapy.
- Evacuation Consideration – Arrange for transport to a higher level of care for worsening symptoms.
This scenario is authored by our VALOR Program. To learn more, see SUC Snake Envenomation.
SUC Ingrown Toenail (Small Unit Care Curriculum)
A patient arrives with toe pain and signs of infection due to an ingrown toenail. Learners must assess the severity and determine whether conservative or procedural management is necessary.
- Physical Examination – Identify signs of infection, granulation tissue, and complications.
- Non-Surgical Management – Implement conservative treatments such as warm soaks and antibiotic therapy.
- Procedure Training – Perform partial nail avulsion when indicated.
- Patient Education – Counsel on prevention strategies and post-treatment care.
This scenario is authored by our VALOR Program. To learn more, see SUC Ingrown Toenail.
Virtual Manikin™ — ENT and Pulmonary (SUC) (Small Unit Care Curriculum)
Simulate a variety of ENT and pulmonary conditions with customizable patient presentations. Learners develop assessment and management skills for common outpatient complaints.
- Flexible Case Selection – Encounter a range of ENT and respiratory disorders.
- Physical Exam & Diagnosis – Perform otoscopy, lung auscultation, and airway assessments.
- Patient Communication – Adjust explanations and care approaches based on patient needs.
- Real-Time Scenario Adjustment – Modify symptoms and findings in response to learner actions.
This scenario is authored by our VALOR Program. To learn more, see Virtual Manikin™ — ENT and Pulmonary (SUC).
Virtual Manikin™ — Abdominal Pain (SUC) (Small Unit Care Curriculum)
Customize an abdominal pain simulation with real-time physiological adjustments. Learners can practice history-taking, physical exam skills, and differential diagnosis formulation in a dynamic case environment.
- Dynamic Patient Response – Adjust vital signs and exam findings based on learner choices.
- Differential Diagnosis Development – Practice recognizing and ruling out emergent conditions.
- Diagnostic Testing – Perform point-of-care imaging and lab evaluations.
- Interdisciplinary Communication – Work with team members to create an effective care plan.
This scenario is authored by our VALOR Program. To learn more, see Virtual Manikin™ — Abdominal Pain (SUC).
Virtual Manikin™ — Prolonged Casualty Care (PCC) (Prolonged Casualty Care Curriculum)
Manage critically injured patients in austere environments where evacuation is delayed. Learners must prioritize limited resources and sustain life over extended periods.
- Prolonged Field Care Principles – Adapt to resource-limited settings and extended patient management.
- Triage & Prioritization – Make critical decisions with constrained medical supplies.
- Team-Based Coordination – Communicate and collaborate under high-stress conditions.
- Long-Term Monitoring – Recognize signs of deterioration and intervene appropriately.
This scenario is authored by our VALOR Program. To learn more, see Virtual Manikin™ — Prolonged Casualty Care (PCC).
PCC Sepsis Management (Prolonged Casualty Care Curriculum)
A critically ill patient presents with fever, hypotension, and altered mental status. Learners must rapidly recognize sepsis and initiate aggressive resuscitation.
- Early Sepsis Recognition – Identify warning signs and initiate rapid response.
- Fluid Resuscitation & Monitoring – Manage hemodynamic stability with IV fluids and vasopressors.
- Infection Source Control – Determine appropriate antibiotic therapy.
- Interdisciplinary Coordination – Work with the critical care team to ensure optimal outcomes.
This scenario is authored by our VALOR Program. To learn more, see PCC Sepsis Management.
PCC Crush Syndrome (Prolonged Casualty Care Curriculum)
A patient trapped under debris is now presenting with signs of crush syndrome. Learners must recognize the condition, prevent complications, and coordinate evacuation.
- Crush Syndrome Identification – Detect early signs of muscle breakdown and systemic effects.
- Electrolyte & Kidney Management – Monitor for hyperkalemia and acute kidney injury.
- Fluid Resuscitation – Administer IV fluids to prevent renal failure.
- Evacuation Readiness – Ensure safe transport while stabilizing the patient.
This scenario is authored by our VALOR Program. To learn more, see PCC Crush Syndrome.
PCC Burn Management (Prolonged Casualty Care Curriculum)
A severely burned patient requires immediate airway protection, fluid resuscitation, and wound care. Learners must stabilize the patient while prioritizing pain control and infection prevention.
- Burn Classification & Assessment – Differentiate between partial and full-thickness burns.
- Airway Protection – Identify inhalation injury and manage accordingly.
- Fluid Resuscitation – Apply the Parkland formula to determine IV fluid needs.
- Pain & Wound Care – Implement analgesia and appropriate dressing techniques.
This scenario is authored by our VALOR Program. To learn more, see PCC Burn Management.
PCC Severe Traumatic Brain Injury (Prolonged Casualty Care Curriculum)
A head trauma patient arrives unconscious with a deteriorating Glasgow Coma Scale score. Learners must stabilize the patient while managing intracranial pressure and preventing secondary injury.
- Neurological Assessment – Perform a focused exam and recognize signs of herniation.
- Intracranial Pressure Management – Implement strategies to prevent worsening brain injury.
- Critical Interventions – Perform airway control and optimize oxygenation.
- Team-Based Care – Communicate effectively with neurosurgery and trauma teams.
This scenario is authored by our VALOR Program. To learn more, see PCC Severe Traumatic Brain Injury.
Scenario Translations
French
- Infant with Bronchiolitis
- Shoulder Dystocia in a Rural ED
German
- PCC Burn Management
- PCC Crush Syndrome
- PCC Sepsis Management
- PCC Severe Traumatic Brain Injury
- Virtual Manikin™ — Prolonged Casualty Care (PCC)
Korean
- Infant with Bronchiolitis
- Shoulder Dystocia in a Rural ED
Spanish
- Chest Pain in the ED (Resuscitation)
- EMS Anaphylaxis
- EMS MCA Stroke
- EMS Motor Vehicle Accident
- EMS Prehospital Pediatric Trauma
- EMS TCA Overdose
- Epileptic Seizure
- GI Bleed
- Infant with Bronchiolitis
- MAT 05 – Amber Rhodes – Preeclampsia, HELLP Syndrome
- MAT 09 – Kaira Abbot – Medical Induction/Fetal Distress
- MAT 14 – Nakita Brown – Fetal Distress/Meconium
- MAT 20 – Maddy Martin – Postpartum Hemorrhage/Vaginal Hematoma
- MAT 21 – Macy Polenski – Postpartum Hemorrhage/Placenta Increta
- Precipitous Labor & Neonatal Resuscitation
- Preeclampsia
- Pediatric Dysrhythmia (Resuscitation)
- Postpartum Hemorrhage in ED
- Sepsis
- Shortness of Breath
- Shoulder Dystocia in a Rural ED
Moderator
Scenario names, authors, and dimensions in SimX 25r1 have been updated to more accurately reflect the goals of each scenario and the relevant organizations.
Scenario Names
- Acute Appendicitis Pre Op – Formerly Known As: Scenario PED 30 – Abdullah Yusuf – Acute Appendicitis, Preoperative
- Acute Appendicitis Post Op – Formerly Known As: Scenario PED 31 – Abdullah Yusuf – Acute Appendicitis / Adolescent / Post-operative Care
- Acute Asthma – Formerly Known As: Scenario PED 24 – Emilia Garcia – Acute Asthma, Management of Impaired Gas Exchange
- Acute Lymphoblastic Leukemia – Formerly Known As: Scenario PED 21 – Suzie Porter – Acute Lymphoblastic Leukemia, Platelet Transfusion
- Acute Myocardial Infarction – Formerly Known As: Estela Rendón – AMI Acute Myocardial Infarction
- Acute Renal Failure – Formerly Known As: Scenario MED 43 – Keola Akana – Acute Renal Failure | Hyperkalemia
- Aggressive Behavior Management for Dementia Patient – Formerly Known As: Aggressive Behavior Management for Patients with Dementia
- Anesthesia Post-op – Formerly Known As: Anesthesia
- Anxiety/Stress Management – Formerly Known As: Scenario PSY 03 – Indira Desai – Anxiety/Stress Management
- Bipolar/Mania – Formerly Known As: Scenario PSY 04 – Jodie Bennett – Bipolar/Mania
- Bleeding Control—Office Shooting – Formerly Known As: Bleeding Control: Office Shooting
- Brief Psychotic Disorders – Formerly Known As: Brief Psychotic Disorders – Mental Health
- C. Diff – Formerly Known As: C-Diff
- Car Accident—Prehospital – Formerly Known As: Multiple Versions: Eenzijdig Verkeersongeval (NLD); Traffic Accident
- Cellulitis and PICC Line Care Skills – Formerly Known As: Med – Surg Nursing Skills
- Chest Pain in the ED (Resuscitation) – Formerly Known As: Chest Pain in the ED
- Chest Pain—ACS – Formerly Known As: Chest pain – ACS
- Coarctation of the Aorta – Formerly Known As: Coarctation
- Community Health Nurse Experience – Formerly Known As: A Community Health Nurse Experience
- COM 01 – Wallace Peterson – Home Visit and COPD Pneumonia – Formerly Known As: Scenario COM 01 – Wallace Peterson – Home Visit and COPD Pneumonia
- COM 02 – Margaret Chan – Home Health – Hospice – Formerly Known As: Scenario COM 02 – Margaret Chan – Home Health – Hospice
- COM 03 – Bradley Wright – Home Health – Heart Failure – Formerly Known As: Scenario COM 03 – Bradley Wright – Home Health – Heart Failure
- COM 04 – Ricky Alvarez – School Health – Diabetic – Formerly Known As: Scenario COM 04 – Ricky Alvarez – School Health – Diabetic
- COM 05 – Emilia Garcia – School Health – Asthma Exacerbation – Formerly Known As: Scenario COM 05 – Emilia Garcia – School Health – Asthma Exacerbation
- COM 06 – Darlene Hall – Public Health – STI – Formerly Known As: Scenario COM 06 – Darlene Hall – Public Health – STI
- COM 07 – Mary Cohen – Occupational Health – Workplace Injury – Formerly Known As: Scenario COM 07 – Mary Cohen – Occupational Health – Workplace Injury
- COM 08 – Kelly Grey – Occupational Health – Stroke/MI Assessment – Formerly Known As: Scenario COM 08 – Kelly Grey – Occupational Health – Stroke/MI Assessment
- COM 09 – Juan Hernandez – Vulnerable Populations – Migrant Farm Worker-Tuberculosis – Formerly Known As: Scenario COM 09 – Juan Hernandez – Vulnerable Populations – Migrant Farm Worker-Tuberculosis
- COM 10 – Tyler Morgan – Vulnerable Populations – Mental Health – Formerly Known As: Scenario COM 10 – Tyler Morgan – Vulnerable Populations – Mental Health
- COM 12 – Community Health – Multiple Casualty Incident – Formerly Known As: Scenario COM 12 – Community Health – Multiple Casualty Incident
- COM 13 – Patient Zero – Community Health – Bioterrorism – Formerly Known As: Scenario COM 13 – Patient Zero – Community Health – Bioterrorism
- Critical Care Post-MVA – Formerly Known As: Critical Care for a Motor Vehicle Crash Victim
- CBRN Civilian Tool Orientation – Formerly Known As: CBRNE Tool Orientation (Civilian)
- CBRN Dirty Bomb Urban Attack – Formerly Known As: CBRNE Dirty Bomb Urban Attack
- CBRN Hydrogen Cyanide Exposure – Formerly Known As: CBRNE Hydrogen Cyanide Exposure
- CBRN Mustard Gas Exposure and Eye Irritation – Formerly Known As: CBRNE Mustard Gas Exposure and Eye Irritation
- CBRN Nerve Agent Exposure Field Decontamination – Formerly Known As: CBRNE Nerve Agent Exposure Field Decon (POI)
- CBRN Nerve Agent Exposure with Severe Head Injury – Formerly Known As: CBRNE Nerve Agent Exposure with Severe Head Injury
- CBRN Opiate Gas Attack – Formerly Known As: CBRNE Opiate Gas Attack
- CBRN Phosgene Oxime (CX) Exposure with Penetrating Trauma – Formerly Known As: CBRNE Phosgene Oxime (CX) Exposure with Penetrating Trauma
- CBRN Radiation Accident with Burn Management – Formerly Known As: CBRNE Radiation Accident with Burn Management
- CBRN Sarin Gas Exposure from IED – Formerly Known As: CBRNE Sarin Gas Exposure from IED
- CBRN Subway Attack with Cyanogen Chloride Exposure – Formerly Known As: CBRNE Subway Attack with Cyanogen Chloride Exposure and Respiratory Failure
- CBRN TIC Exposure with Blunt Traumatic Injuries – Formerly Known As: CBRNE TIC Exposure with Blunt Traumatic Injuries
- CBRN TIC Exposure with Blunt Traumatic Injuries Civilian Response – Formerly Known As: CBRNE TIC Exposure with Blunt Traumatic Injuries (Civilian)
- CBRN Tool Orientation – Formerly Known As: CBRNE Tool Orientation (Military)
- Virtual Manikin™ — Chemical Exposure (CBRN) – Formerly Known As: CBRNE Virtual Manikin – Chemical Exposure
- De-escalation of Agitated Patient – Formerly Known As: Agitation
- Dementia – Formerly Known As: Scenario PSY 10 – Ri Liang – Dementia
- Depression – Formerly Known As: Scenario PSY 01 – Cecil Whitver – Depression
- Difficult Client – Formerly Known As: Difficult Client Interaction
- Domestic Violence – Formerly Known As: Scenario HA 3-3 – Mary Cohen – Domestic Violence
- Drug Abuse – Formerly Known As: Scenario PSY 05 – Tyler Morgan – Drug Abuse
- EMS Anaphylaxis – Formerly Known As: Anaphylaxis EMS
- EMS Anaphylaxis with Difficult Airway – Formerly Known As: EMS: Anaphylactic Respiratory Failure
- EMS Climbing Accident and Rescue – Formerly Known As: Wilderness Climbing Accident
- EMS Combative—Suicidal Intent – Formerly Known As: EMS: Combative Suicidal Intent
- EMS Congestive Heart Failure – Formerly Known As: EMS: Congestive Heart Failure
- EMS Diabetic Emergency – Formerly Known As: EMS: Diabetic Emergency
- EMS Inferior STEMI – Formerly Known As: Inferior STEMI EMS
- EMS MCA Stroke – Formerly Known As: SimX EMS MCA Stroke Team Activation in Field
- EMS Motor Vehicle Accident – Formerly Known As: 40 yo M MVA – ATLS
- EMS Obstetrics Emergency – Formerly Known As: EMS: Obstetrics Emergency
- EMS Pediatric Hypovolemic Shock – Formerly Known As: EMS: Pediatric Hypovolemic Shock
- EMS Pediatric Overdose – Formerly Known As: EMS: Pediatric Overdose
- EMS Pool Accident – Formerly Known As: EMS: Pool Accident
- EMS Prehospital Pediatric Trauma – Formerly Known As: EMS Pediatric Patient with Trauma
- EMS TCA Overdose – Formerly Known As: TCA OD
- EMS Trauma—Electrocution – Formerly Known As: EMS: Trauma – Electrocution
- EMS Trauma—Stabbing – Formerly Known As: EMS: Trauma – Stabbing
- Epileptic Seizure – Formerly Known As: Bern SAH
- Fall in the Hospital – Formerly Known As: Fall
- Goals of Care Discussion – Formerly Known As: Goals of Care Discussion – Soliciting Values from Family
- Geriatric Pneumonia—Inpatient – Formerly Known As: Pneumonia
- HA 1-4 – Christina Brown – Contraception Initiation – Young Adult Female – Formerly Known As: Scenario HA 1-4 – Christina Brown – Contraception Initiation – Young Adult Female
- HA 3-1 – Mary Cohen – Nursing Admission – Female – Formerly Known As: Scenario HA 3-1 – Mary Cohen – Nursing Admission – Female
- HA 9-1 – Marc Kozlov – Post-operative Respiratory Distress – Formerly Known As: Scenario HA 9-1 – Marc Kozlov – Post-operative Respiratory Distress
- Hypoglycemic Shock – Formerly Known As: Senior Level Hypoglycemic Shock
- Infant with Bronchiolitis – Formerly Known As: Bronchiolitis – PALS Scenario
- Interprofessional Gender-Affirming Care in an Adult – Formerly Known As: Interprofessional Care for Katarina
- Intubation of Pediatric Patient with Suspected COVID – Formerly Known As: Intubation of the Suspected or Confirmed COVID Patient
- LED 01 – Margaret Chan – Medication Error RCA – Formerly Known As: Scenario LED 01 – Margaret Chan – Medication Error RCA
- LED 02 – Susan Weil – Respiratory Distress/Rapid Response – Formerly Known As: Scenario LED 02 – Susan Weil – Respiratory Distress/Rapid Response
- LED 03 – Managing Care of Multiple Patients – Formerly Known As: Scenario LED 03 – Managing Care of Multiple Patients
- Lumbar Radiculopathy – Formerly Known As: Right L5 Radiculopathy
- MAT 01 – Darlene Hall – Intimate Partner Violence – Formerly Known As: Scenario MAT 01 – Darlene Hall – Intimate Partner Violence
- MAT 02 – Jessie Baer – Insulin-Dependent Gestational Diabetes/Preterm Labor – Formerly Known As: Scenario MAT 02 – Jessie Baer – Insulin-Dependent Gestational Diabetes/Preterm Labor
- MAT 03 – Meagan Solitas – Late Pregnancy Bleeding/Placenta Previa – Formerly Known As: Scenario MAT 03 – Meagan Solitas – Late Pregnancy Bleeding/Placenta Previa
- MAT 04 – Becca Roberts – Hyperemesis Gravidarum – Formerly Known As: Scenario MAT 04 – Becca Roberts – Hyperemesis Gravidarum
- MAT 05 – Amber Rhodes – Preeclampsia, HELLP Syndrome – Formerly Known As: Scenario MAT 05 – Amber Rhodes – Preeclampsia, HELLP Syndrome
- MAT 06 – Rona Berends – Preeclamptic Seizure – Formerly Known As: Scenario MAT 06 – Rona Berends – Preeclamptic Seizure
- MAT 07 – Carole Shotz – Scheduled Cesarean Delivery – Formerly Known As: Scenario MAT 07 – Carole Shotz – Scheduled Cesarean Delivery
- MAT 08 – Abby Frank – Fetal Demise, Induction – Formerly Known As: Scenario MAT 08 – Abby Frank – Fetal Demise, Induction
- MAT 09 – Kaira Abbot – Medical Induction/Fetal Distress – Formerly Known As: Scenario MAT 09 – Kaira Abbot – Medical Induction/Fetal Distress
- MAT 10 – Kaelyn Renard – Intrapartal Infection – Formerly Known As: Scenario MAT 10 – Kaelyn Renard – Intrapartal Infection
- MAT 11 – Diana Akita-Byrd – Birth Plan Change – Formerly Known As: Scenario MAT 11 – Diana Akita-Byrd – Birth Plan Change
- MAT 13 – Reanne Zoller – Post-Term Birth/Distress/Meconium – Formerly Known As: Scenario MAT 13 – Reanne Zoller – Post-Term Birth/Distress/Meconium
- MAT 14 – Nakita Brown – Fetal Distress/Meconium – Formerly Known As: Scenario MAT 14 – Nakita Brown – Fetal Distress/Meconium
- MAT 15 – Danica Crowley – Neonatal Resuscitation, Narcotic – Formerly Known As: Scenario MAT 15 – Danica Crowley – Neonatal Resuscitation, Narcotic
- MAT 16 – Haley Bellows – Neonatal Resuscitation/Cardiac Anomaly – Formerly Known As: Scenario MAT 16 – Haley Bellows – Neonatal Resuscitation/Cardiac Anomaly
- MAT 17 – Maria Fernando – Shoulder Dystocia, Neonatal Resuscitation – Formerly Known As: Scenario MAT 17 – Maria Fernando – Shoulder Dystocia, Neonatal Resuscitation
- MAT 18 – Deborah Nelson – Newborn Care – Formerly Known As: Scenario MAT 18 – Deborah Nelson – Newborn Care
- MAT 19 – Stacey Downes – Postpartum Hemorrhage/Uterine Atony – Formerly Known As: Scenario MAT 19 – Stacey Downes – Postpartum Hemorrhage/Uterine Atony
- MAT 20 – Maddy Martin – Postpartum Hemorrhage/Vaginal Hematoma – Formerly Known As: Scenario MAT 20 – Maddy Martin – Postpartum Hemorrhage/Vaginal Hematoma
- MAT 21 – Macy Polenski – Postpartum Hemorrhage/Placenta Increta – Formerly Known As: Scenario MAT 21 – Macy Polenski – Postpartum Hemorrhage/Placenta Increta
- MED 02 – Wallace Peterson – Pneumonia with Acute Respiratory Distress and Oxygen Delivery – Formerly Known As: Scenario MED 02 – Wallace Peterson – Pneumonia with Acute Respiratory Distress and Oxygen Delivery
- MED 04 – Kimberly Dunning – Asthma Exacerbation & Anxiety, Communication & Oxygen Delivery – Formerly Known As: Scenario MED 04 – Kimberly Dunning – Asthma Exacerbation & Anxiety, Communication & Oxygen Delivery
- MED 05 – Margaret Chan – Lung Cancer, Nausea & Hypokalemia – Formerly Known As: Scenario MED 05 – Margaret Chan – Lung Cancer, Nausea & Hypokalemia
- MED 08 – Ricardo Mendoza – Lung Cancer and Acute Tension Pneumothorax – Formerly Known As: Scenario MED 08 – Ricardo Mendoza – Lung Cancer and Acute Tension Pneumothorax
- MED 09 – Keola Akana – Heart Failure/Digoxin Toxicity & Hypokalemia – Formerly Known As: Scenario MED 09 – Keola Akana – Heart Failure/Digoxin Toxicity & Hypokalemia
- MED 11 – Melody Dixon – Myocardial Infarction and Management of Unstable Patient – Formerly Known As: Scenario MED 11 – Melody Dixon – Myocardial Infarction and Management of Unstable Patient
- MED 18 – David Montanari – Spinal Cord Injury and Postoperative Atelectasis – Formerly Known As: Scenario MED 18 – David Montanari – Spinal Cord Injury and Postoperative Atelectasis
- MED 23 – Lou Thao – Abdominal Surgery and Patient Controlled Analgesia – Formerly Known As: Scenario MED 23 – Lou Thao – Abdominal Surgery and Patient Controlled Analgesia
- MED 24 – Lou Thao – Abdominal Surgery and Postoperative Fluid Volume Deficit – Formerly Known As: Scenario MED 24 – Lou Thao – Abdominal Surgery and Postoperative Fluid Volume Deficit
- MED 26 – Lucia Hoyos – Colostomy and Hyperkalemia Secondary to Medication Error – Formerly Known As: Scenario MED 26 – Lucia Hoyos – Colostomy and Hyperkalemia Secondary to Medication Error
- MED 28 – Cynthia Bennet – Urinary Tract Infection and Anaphylactic Reaction – Formerly Known As: Scenario MED 28 – Cynthia Bennet – Urinary Tract Infection and Anaphylactic Reaction
- MED 29 – Taylor Westfield – Gastrointestinal Bleed – Formerly Known As: Scenario MED 29 – Taylor Westfield – Gastrointestinal Bleed
- MED 33 – Arthur Harris – Diabetes – Severe Acute Hypoglycemia – Formerly Known As: Scenario MED 33 – Arthur Harris – Diabetes – Severe Acute Hypoglycemia
- MED 35 – Janet Owen – Pancreatitis and Alcohol Withdrawal – Formerly Known As: Scenario MED 35 – Janet Owen – Pancreatitis and Alcohol Withdrawal
- MED 37 – Susan Weil – Hip Fracture and Blood Transfusion – Formerly Known As: Scenario MED 37 – Susan Weil – Hip Fracture and Blood Transfusion
- MED 38 – Susan Weil – Hip Fracture and Pulmonary Embolism – Formerly Known As: Scenario MED 38 – Susan Weil – Hip Fracture and Pulmonary Embolism
- MED 40 – Agnes Taylor – Hip Fracture, Wound Infection & Early Sepsis – Formerly Known As: Scenario MED 40 – Agnes Taylor – Hip Fracture, Wound Infection & Early Sepsis
- MED 41 – Mathias Hedding – Wound Debridement and Pain Management – Formerly Known As: Scenario MED 41 – Mathias Hedding – Wound Debridement and Pain Management
- MED 43 – Keola Akana – Acute Renal Failure | Hyperkalemia – Formerly Known As: Scenario MED 43 – Keola Akana – Acute Renal Failure | Hyperkalemia
- MED 45 – Matt Slattery – Hemothorax with Chest Tube and Drug Overdose – Formerly Known As: Scenario MED 45 – Matt Slattery – Hemothorax with Chest Tube and Drug Overdose
- Myocardial Infarction in the ED – Formerly Known As: Myocardial Infarction
- New-onset Type 2 Diabetes in Adult – Formerly Known As: Diabetes
- Non-Fatal Suicide Attempt in an Adult – Formerly Known As: Mental Health/Failed Suicide Attempt/Suicidal Ideation/Depression
- Outpatient Preeclampsia – Formerly Known As: Preeclampsia
- PCC Burn Management – Formerly Known As: PCC: Burn Management
- PCC Crush Syndrome – Formerly Known As: PCC: Crush Injury
- PCC Sepsis Management – Formerly Known As: PCC: Sepsis Management
- PCC Severe Traumatic Brain Injury – Formerly Known As: PCC: Severe Traumatic Brain Injury
- Pediatric Asthma Exacerbation – Formerly Known As: Pediatric Asthma Exacerbation
- Pediatric Dysrhythmia (Resuscitation) – Formerly Known As: PALS – 9 y/o Collapse During PE
- Pediatric Low Cardiac Output Syndrome – Formerly Known As: Low Cardiac Output Syndrome / Junctional Ectopic Tachycardia
- Pediatric Post-op Hypoxia and Hypotension – Formerly Known As: Hypoxia and Hypotension in a Post-op Stage 1 Palliation (Norwood Procedure)
- Pediatric Post-op SVT – Formerly Known As: Post-op SVT
- Pediatric Pulmonary Hypertensive Crisis – Formerly Known As: Pulmonary Hypertensive Crisis
- Pediatric Sepsis – Formerly Known As: Sepsis
- Pediatric Tonsil and Adenoid – Formerly Known As: Pediatric Tonsil and Adenoid Post-Operative
- Post-op Mobility and Elimination – Formerly Known As: Mobility and Elimination Simulation Case 1
- Postpartum Depression – Formerly Known As: Postpartum Follow-Up – Depression Screening – Culturally Diverse Non-English Speaking Patient
- Postpartum Hemorrhage in ED – Formerly Known As: Postpartum Hemorrhage
- Postpartum Hemorrhage—Hospital – Formerly Known As: Postpartum Hemorrhage
- Precipitous Labor & Neonatal Resuscitation – Formerly Known As: Precipitous Labor & NRP
- Primary Care COVID-19 – Formerly Known As: Primary Care – Home Health COVID
- Primary Postpartum Hemorrhage – Formerly Known As: Primary Postpartum Haemorrhage
- Prioritization of Multiple Patients – Formerly Known As: Prioritization
- PSY 08 – Jessie Hernandez – Post-traumatic Stress Disorder – Formerly Known As: Scenario PSY 08 – Jessie Hernandez – Post-traumatic Stress Disorder
- PSY 09 – Marcie Anderson – Obsessive Compulsive Disorder – Formerly Known As: Scenario PSY 09 – Marcie Anderson – Obsessive Compulsive Disorder
- PSY 10 – Ri Liang – Dementia – Formerly Known As: Scenario PSY 10 – Ri Liang – Dementia
- PSY 11 – Tessa Walker – Personality Disorder – Formerly Known As: Scenario PSY 11 – Tessa Walker – Personality Disorder
- PSY 12 – Gwen Harrison – Older Adult Abuse – Formerly Known As: Scenario PSY 12 – Gwen Harrison – Older Adult Abuse
- Sepsis – Formerly Known As: ED Sepsis
- Sepsis Care – Formerly Known As: Sepsis
- Shortness of Breath – Formerly Known As: COVID-19 ED Evaluation
- Shoulder Dystocia in a Rural ED – Formerly Known As: High-Risk OB
- STEMI V-Fib Arrest – Formerly Known As: STEMI VFib Arrest
- SUC Abdominal Pain – Formerly Known As: SUC: Abdominal Pain
- SUC Cold-Related Illness – Formerly Known As: SUC: Cold-Related Illness
- SUC Deep Venous Thrombosis – Formerly Known As: SUC: Deep Venous Thrombosis
- SUC Flank Pain – Formerly Known As: SUC: Flank Pain
- SUC Ingrown Toenail – Formerly Known As: SUC: Ingrown Toenail
- SUC Peritonsillar Abscess – Formerly Known As: SUC: Peritonsillar Abscess
- SUC Rhabdomyolysis – Formerly Known As: SUC: Rhabdomyolysis
- SUC Snake Envenomation – Formerly Known As: SUC: Snake Envenomation
- Suicidal Risk Assessment – Formerly Known As: Suicide Assessment of a Mental Health Patient
- Teenager with Chest Pain – Formerly Known As: Chest Pain
- Triage Mass Casualty – Formerly Known As: Multiple Versions: Explosion with Multiple Victims (ENG); Explosie Met Meerdere Gewonden (NLD)
- Tracheostomy Complications—Chronic Tracheostomy with Tracheoinnominate Fistula – Formerly Known As: Tracheostomy Complications – Chronic Tracheostomy with Tracheoinnominate Fistula
- Tracheostomy Complications—Cuff Leak – Formerly Known As: Tracheostomy Complications – Cuff Leak
- Tracheostomy Complications—Displacement (Fresh Total Laryngectomy) – Formerly Known As: Tracheostomy Complications – Displacement (Fresh Total Laryngectomy)
- Tracheostomy Complications—Occluded Inner Cannula (Fresh Tracheostomy) – Formerly Known As: Tracheostomy Complications – Occluded Inner Cannula (Fresh Tracheostomy)
- Virtual Manikin™ — Abdominal Pain (SUC) – Formerly Known As: SUC: Virtual Manikin – Abdominal Pain
- Virtual Manikin™ — Adult Chest Pain – Formerly Known As: Virtual Manikin – Adult Chest Pain
- Virtual Manikin™ — Chemical Exposure (CBRN) – Formerly Known As: CBRNE Virtual Manikin – Chemical Exposure
- Virtual Manikin™ — ENT and Pulmonary (SUC) – Formerly Known As: SUC: Virtual Manikin – ENT and Pulmonary
- Virtual Manikin™ — Outpatient Soft Skills – Formerly Known As: Virtual Manikin: Outpatient Soft Skills
- Virtual Manikin™ — Pediatric Respiratory – Formerly Known As: Virtual Manikin – Pediatric Respiratory
- Virtual Manikin™ — Prolonged Casualty Care (PCC) – Formerly Known As: PCC: Virtual Manikin
- Workplace Violence & De-escalation – Formerly Known As: VR Interprofessional Simulation Training on Responding to Workplace Violence
Authors
- Eastern Michigan University School of Nursing – Formerly Known As: Eastern Michigan
- Indiana University East School of Nursing and Health Sciences – Formerly Known As: IU East
- Indiana University School of Nursing – Formerly Known As: IUPUC
- Inselspital – Universitätsspital Bern – Formerly Known As: Inselspital
- Keimyoung University – Formerly Known As: Dymstec
- Maimonides Medical Center – Formerly Known As: Maimonides
- Mount Saint Mary’s University – Formerly Known As: Mount Saint Mary
- Nambu University – Formerly Known As: Dymstec
- Ohio State University – Formerly Known As: Ohio State
- Queensland Health Service – Formerly Known As: Bundle of Rays
- Servicio Nacional de Aprendizaje (SENA) – Formerly Known As: TM Medica
- South Carolina State University – Formerly Known As: SCSU
- Sun City Simulation – Formerly Known As: Sun City
- University of Nebraska Medical Center School of Nursing – Formerly Known As: UNMC
- University of Pennsylvania School of Nursing – Formerly Known As: UPenn
- VALOR Program – Formerly Known As: SimX VALOR
- XR Support Center Europe – Formerly Known As: VR Support Center Europe
Room Dimensions
New:
- The moderator now shows room dimensions in units of (ft) and (m).
- All room dimensions have been updated with accurate measurements.